Low back pain and neck pain are one of the most common reasons for seeking medical attention. Pain is usually caused by problems with the musculoskeletal system - most pronounced with problems with the spine, including the bones of the spine (vertebrae), discs, and the muscles and ligaments that support them. Sometimes back pain is caused by a condition that does not affect the musculoskeletal system.
Low back pain is more common in older age groups, affecting more than half of people over the age of 60. It leads to significant costs in terms of health care payments, disability benefits and missed work hours due to illness.
The spine (vertebral column) is made up of vertebrae. There are shock-absorbing discs between the vertebrae. Discs have a tough outer layer of fibrocartilaginous tissue and a soft, jelly-like inner substance called a nucleus. Each vertebra has two joints behind the discs. These joints are called facet joints. The articular surfaces of one vertebral body lie on the articular surfaces of the other under it, forming a joint. The joints, and with them the entire spine, are stabilized by ligaments and muscles, namely:
- Two iliopsoas muscles that run on either side of the spine
- Two erector muscles of the back that run the entire length of the spine behind it
- Many short paravertebral muscles located between the vertebrae
The spinal cord is located in the spinal canal. Along the entire length of the spinal cord, through the holes between the vertebrae on both sides, the spinal nerves exit, the function of which is to unite all the nerves in the body. The part of the spinal nerve near the spinal cord is called the root. Due to the peculiarities of the position of the roots of the spinal nerves, they can be compressed (compression) with injuries of the spine, which leads to pain.
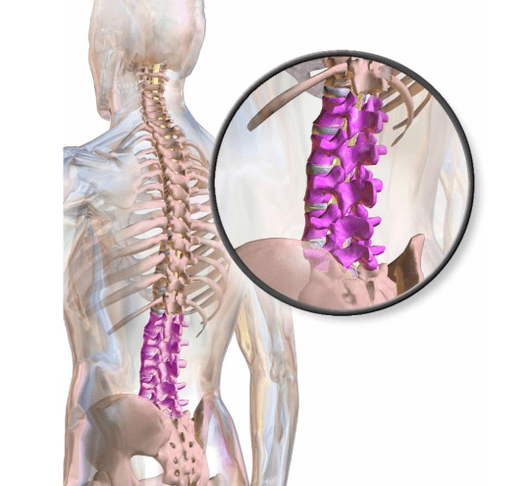
The lower spine (lumbar spine) at the top connects to the upper spine (thoracic spine) and below the pelvis through the sacrum bone. The lumbar spine is flexible enough to bend, twist, and bend, and provides strength while standing, walking and lifting. Thus, the lower back is involved in almost all daily activities. Low back pain can interfere with various activities and worsen the quality of life.
Types of back pain
Common types of low back pain include localized, radiating, and repercussion pain.
Local painappears in a certain area of the lower back. It is the most common type of back pain. The cause is usually a disc injury, arthritis of the joint, and, less commonly, a muscle strain. The pain can be continuous and aching, or at some point alternate with intermittent acute pain. Sudden pain can appear when trauma is the cause. Local pain can increase or decrease with a change in position. Touching the lower back can be painful. Muscle spasms are possible.

Radiating painIs low back pain that spreads to the leg. The pain can be dull or sharp and intense. Typically, it affects only the side or back of the leg and can extend to the foot or just to the knee. Radiating pain is usually a manifestation of compression of the spinal nerve root in disorders such as a herniated disc, sciatica, osteoarthritis, or spinal stenosis. Coughing, sneezing, straining, or bending with your legs straight can be painful. When a spinal nerve root is compressed, pain may be accompanied by weakness in the leg muscles, a tingling sensation, or even loss of sensation. In rare cases, loss of control of urination (urinary incontinence) or loss of control over bowel movements (fecal incontinence) occurs.
Reflected painfelt in a place other than the actual cause of the pain. For example, some people with a heart attack feel pain in their left arm. The reflected pain from the internal organs in the lower back is predominantly deep and aching in nature, and its exact localization is difficult to determine. As a rule, with movement, the pain does not increase, in contrast to the pain accompanying disorders of the musculoskeletal system.
The reasons
In most cases, back pain is a consequence of diseases of the spine and surrounding joints, muscles, ligaments and roots of the spinal nerves, as well as intervertebral discs. Often, a single specific cause cannot be identified. Any painful spinal disease can lead to reflex contraction (spasm) of the muscles around the spine. The spasm may increase the pain. Stress can make lower back pain worse, but the mechanism is not clear.
Sometimes, back pain is caused by a disorder that does not affect the spine, such as cancer, gynecological conditions (such as premenstrual syndrome), kidney disease (such as kidney stones), urinary tract disease (such as infections of the kidneys, bladder, and prostate)and the digestive tract (for example, diverticulitis), as well as diseases of the large arteries located near the spine.
Common Causes
Common causes of back pain include the following:
- Osteoarthritis
- Compression fractures of the spine
- A ruptured or herniated intervertebral disc
- Spinal stenosis in the lumbar spine
- Spondylolisthesis
- Damage to muscles and ligaments
- Fibromyalgia
Damagecan occur during normal activities (for example, lifting heavy objects, exercising, unexpected movement) or as a result of injury, such as a fall or traffic accident. Typically, imaging studies do not show any specific lesions, but doctors suspect that some muscles and / or ligaments are affected.
Osteoarthritis(degenerative arthritis) causes wear and tear of the cartilage between the articular surfaces and the formation of bone spines (osteophytes). This disease is partly the result of years of tissue wear. With severe degeneration and loss of disc height, osteophytes in the foramen can compress the spinal nerve roots. All of these changes can lead to lower back pain as well as stiffness.
Compression fractures of the spine (due to compression)(vertebral fractures) often occur when bone density decreases due to osteoporosis, which usually develops with age. However, fractures due to osteoporosis tend to occur in the upper and middle back and are accompanied by pain in these regions rather than in the lower spine.
A ruptured or herniated intervertebral disccan cause back pain. The disc is represented by a dense outer layer and a soft, jelly-like central part. If the disc is under constant stress from the vertebrae above and below (for example, when bending forward, especially when lifting heavy objects), its outer layer can break (tear), causing pain.
Spinal stenosis in the lumbar spine- Narrowing of the spinal canal (which runs through the center of the spine and contains the spinal cord and the bundle of nerves that extend downward from the lower part of the spinal cord) in the lumbar region. It is a common cause of low back pain in older people. Spinal stenosis also develops in middle age in people whose spinal canal is narrow from birth. Spinal stenosis is caused by disorders such as osteoarthritis, spondylolisthesis, ankylosing spondylitis, and Paget's disease.
Spinal stenosis can cause sciatica as well as back pain.
Spondylolisthesis- partial displacement of the vertebra in the lower part of the spine. One type usually occurs during adolescence or adolescence (often in athletes) and is caused by an injury that fractures a portion of the vertebrae. If both sides of the vertebra are affected, the vertebra can slide forward over the underlying vertebra. Spondylolisthesis can also occur in the elderly, but mainly as a result of degenerative disease. With the development of spondylolisthesis in adulthood, the risk of spinal stenosis in the lumbar region increases.
FibromyalgiaIs a common cause of pain that affects many parts of the body, including the lower back. This condition results in chronic diffuse pain in the muscles and other soft tissues outside the lower back. Fibromyalgia is also characterized by sleep disturbances and fatigue.
Surveys
Tests are usually not prescribed because most back pain is due to osteoarthritis, sprains, or other minor musculoskeletal disorders and resolves within 6 weeks. Imaging tests are often needed if:
- another reason is suspected;
- there are warning signs;
- back pain persists.
Evaluation may also be ordered if there is no response to initial treatment, or if symptoms worsen or change.
X-rays of the lower back can only provide an image of the bones. Such images can detect degenerative changes due to osteoarthritis, spinal compression fractures, spondylolisthesis, and ankylosing spondylitis. However, magnetic resonance imaging (MRI) or computed tomography (CT) can provide a clear image of bones and, as is typical for MRI, display soft tissue (including discs and some nerves). An MRI or CT scan is usually needed when doctors determine the presence of disorders that lead to some changes in the structure of bones, as well as soft tissue diseases.
If spinal cord compression is suspected, MRI is done as soon as possible. In the rare cases where MRI results are ambiguous, CT myelography may be necessary. Rarely, if a malignant tumor or infection is suspected, a tissue sample (biopsy) needs to be taken for analysis. In some cases, electromyography and examinations to study nerve conduction are performed to confirm the presence, localization and, in some cases, the duration and severity of the compression of the spinal nerve root.
Prevention
People can reduce their risk of developing low back pain by taking the following measures:
- physical exercises;
- exercises to strengthen and stretch muscles;
- maintaining normal body weight;
- maintaining correct posture;
- compliance with recommendations for safe lifting of weights.
The most effective method of preventing low back pain is through regular exercise. Aerobic exercise and special exercises for the development of muscle strength and stretching are advisable.
Aerobic exercise, such as swimming and walking, improves overall fitness and strengthens muscles.
Special exercises for developing muscle strength and stretching the muscles of the abdominal wall, buttocks and back (deep muscles of the trunk), allow you to stabilize the spine and reduce the stretching of the discs that absorb the spine and the ligaments that hold them.
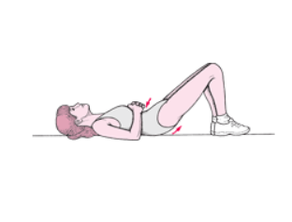
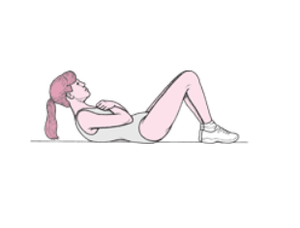
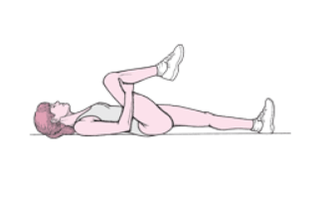
Strength-building exercises include pelvic tilts and abdominal crunches. Stretching exercises include stretching by bending the knees to the chest. In some people, stretching exercises can lead to increased back pain, so caution should be exercised. The basic rule is that any exercise that causes or worsens back pain must be stopped. Exercises should be repeated until mild (but not extreme) muscle fatigue is felt. Breathing is essential during exercise. People with back pain should consult a doctor before exercising.
Pelvic tilts Lie on your back, knees bent, heels on the floor, load on the heels. Press your back to the floor, tense your glutes (lift them about half an inch off the floor) and tense your abdominal muscles. Hold this position for a count of 10. Repeat 20 times. |
 |
Lying crunches Lie on your sleep with your knees bent and your feet flat on the floor. Fold your arms over your chest. Tighten your abdominal muscles, slowly lift your shoulders about 10 inches off the floor, keeping your head straight (your chin should not touch your chest). Relax your abdominal muscles, slowly lower your shoulders. Do 3 sets of 10 reps. |
 |
Stretches with the knees to the chest Take a supine position, straighten up. Place both palms under one knee and press it to your chest. Hold the position for a count of 10. Slowly lower your leg and repeat the exercise on the other leg. Do the exercise 10 times. |
 |
Exercise also makes it easier to maintain your desired body weight. Exercise also helps maintain bone density. Thus, exercise can reduce the risk of developing two conditions that can cause low back pain: obesity and osteoporosis.
Correct posture while standing and sitting reduces stress on the back. Slouching should be avoided. Chair seats should be adjusted in height so that the feet are flat on the floor, the knees are slightly bent, and the lower back is snug against the back of the chair. If the chair does not provide support for the lower back, a pillow can be placed under it. In a sitting position, it is recommended to put your feet on the floor, not cross your legs. People who are sick should not stand or sit for extended periods. If you have to stand or sit for a long time, frequent position changes can reduce the strain on your back.
Treatment
If it is possible to determine a specific cause, the disease is treated. For example, antibiotics are used to treat a prostate infection. However, there is no cure for sprain pain in the musculoskeletal system, or pain caused by other conditions. However, the situation can be improved through general measures. Typically, such measures are also used when squeezing the spinal nerve root.
General measures for back pain
Possible measures include:
- Making changes to activities
- Taking pain relievers
- Applying heat or cold to the painful area
- Light exercise, if tolerated
For more recent back pain, treatment begins by eliminating activities that strain the back and cause pain, such as lifting weights and bending. Bed rest does not accelerate pain relief, and most professionals recommend doing light work. Bed rest, which is necessary to relieve severe pain, should not last more than 1 or 2 days. Prolonged bed rest weakens the core muscles and increases stiffness, leading to worse back pain and slower recovery. Corsets and traction are ineffective. Traction can slow down healing.
Over-the-counter or prescription non-steroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Opioid analgesics are sometimes prescribed if NSAIDs do not provide sufficient pain relief, but they should only be used for a short time, as long-term use of opioid analgesics may, conversely, increase sensitivity to pain, cause side effects, and increase the risk of addiction and dependence.
Muscle relaxants can sometimes relieve muscle spasms, but their effectiveness is questionable. These drugs are not recommended for older patients who are more likely to develop side effects such as drowsiness and confusion. Doctors try not to prescribe muscle relaxants if the patient does not have visible and palpable muscle spasms. If muscle relaxants are prescribed, they should not be used for more than 72 hours. Doctors sometimes recommend taking them just before bed.
Massage can provide some temporary relief from lower back pain. Some studies have shown positive results from acupuncture; others have contradicted these findings. Spine manipulation by chiropractors or other doctors (such as osteopathic doctors), combined with an exercise program, can also relieve pain. However, manipulation of the spine can increase the risk of additional injury and should be avoided in individuals with inflammatory arthritis, neck problems that cause cervical instability, or herniated spinal discs.
It is recommended to sleep in a comfortable position on a medium firm mattress. People who sleep on their backs should have a pillow under their knees. Patients who sleep on their side should use a pillow that allows their head to be kept in a neutral position (without bending the neck up or down). Patients should place a second pillow between the knees, with knees and hips slightly bent, if this relieves lower back pain. Patients can still sleep on their stomachs if they feel comfortable.
Continue or start taking other preventive measures (correct posture, proper weight lifting technique). When carrying out such events, attacks of back pain mostly disappear in the period from several days to 2 weeks. Regardless of the treatment, 80 to 90% of these attacks resolve within 6 weeks.
Treatment of chronic low back pain
Additional measures are needed to treat chronic low back pain. Aerobic exercise is advisable, and weight loss is recommended if necessary. If analgesics are ineffective, other treatments should be prescribed.
Transcutaneous electroneurostimulation (TENS) is possible. CHENS devices generate a weak alternating current that causes a slight tingling sensation. This current can block the transmission of some pain sensations from the spinal cord to the brain. The current can be applied to the painful area several times a day, the duration of the session ranges from 20 minutes to several hours, depending on the severity of the pain.
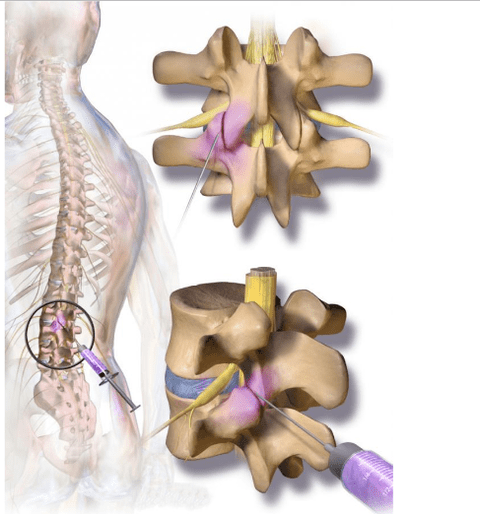
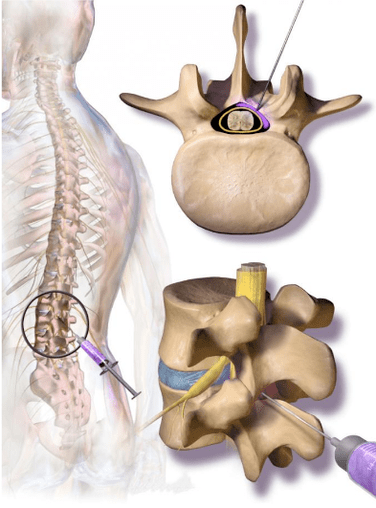
Sometimes corticosteroids with a local anesthetic are periodically injected into the facet joint of the spine or into the epidural space - between the spine and the outer layer of tissue covering the spinal cord. Epidural injections may be more effective for sciatica, which results from a herniated disc rather than lumbar spinal stenosis. However, they may not have long-term beneficial effects. They usually last only a few days or weeks. Their main purpose is to relieve pain so that you can exercise for long-term pain relief.
Back pain surgery
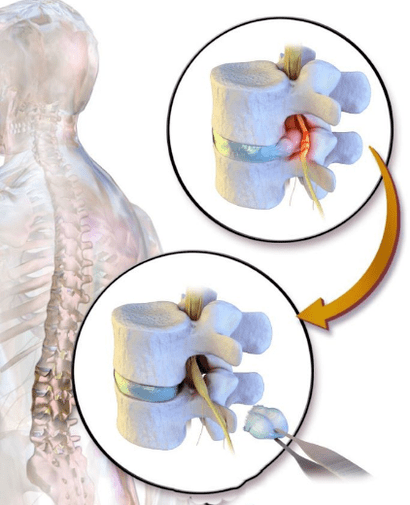
In cases where a herniated disc leads to persistent or chronic sciatica, weakness, loss of sensitivity or fecal and urinary incontinence, it may be necessary to surgically remove the protruding part of the disc (discectomy) and, in some cases, part of the vertebra (laminectomy).
In severe spinal stenosis, a large portion of the posterior vertebra (lamellae of the vertebral arch) may be removed to expand it (lumbar laminectomy). General anesthesia is usually needed. The length of hospital stay is usually 4 to 5 days. Patients will be able to return to normal activities in 3-4 months. Adequate or complete recovery is observed in about two-thirds of patients. For the rest of patients, such surgery can prevent pain and worsening of other symptoms.
If the spine is unstable (which can result from a severe herniated disc, spondylolisthesis, or laminectomy for spinal stenosis), surgery may be performed to fusion the vertebrae (called arthrodesis of the lumbar vertebrae). However, fusion restricts mobility, can be accompanied by excessive mechanical stress on the rest of the spine, and cause problems in the future.
Compression fractures of the spine
Compression fractures of the spine are quite common in women over 50. They can be treated conservatively without surgery, with braces, pain relievers, and possibly calcitonin nasal spray, which will not help bone healing but may reduce pain.
If sufficient pain control cannot be achieved, two surgical options are available:
- Vertebroplasty: the injection of cement mortar into a broken bone.
- Kyphoplasty: Inserting a balloon into a fractured bone to create space. The balloon is then filled with cement.
However, recent studies have shown that in the long term, the effectiveness of these surgical procedures does not outweigh the effectiveness of non-surgical treatment options.
Key points
- Low back pain is common. It is usually caused by musculoskeletal disorders of the spine and factors such as fatigue, obesity and lack of physical activity.
- Low back pain is rarely severe at a young age and testing is usually unnecessary unless symptoms persist for many weeks.
- Patients with warning signs or patients over the age of 55 should see a doctor immediately.
- Strengthening the muscles of the abdominal wall and back with specific exercises helps prevent the most common types of low back pain.
- For back pain, most often, sufficient treatment is to exclude measures leading to mechanical effects on the back, take painkillers, and, in some cases, apply a cold or warm compress.
- Prolonged bed rest and stretching can slow down recovery.
- In severe cases, such as abnormal sensations and weakness in the legs, surgery may be required.
- Compression fractures of the vertebrae can be treated conservatively (with braces, pain relievers and nasal spray) or, in some cases, more aggressively with surgery.



































